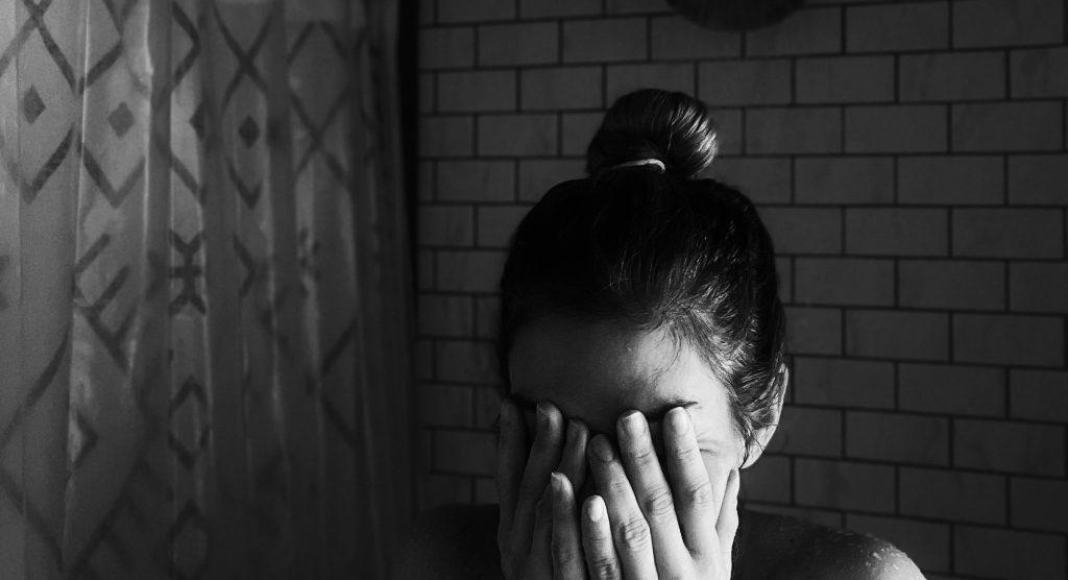
Content Warning: Mention of intrusive thoughts, postpartum anxiety/depression/OCD.
 A few days after I got that first positive pregnancy test, I ran to my local Barnes & Noble to pick up a few books to help me prepare. Then I placed an Amazon order for a few more books. I bought books on pregnancy, breastfeeding, labor/delivery, pumping, and parenting skills. Initially, I struggled with some severe insomnia, so I spent many late nights googling and reading about every plausible scenario that could play out over the next nine months. I even made an illustrated guide on how to care for a newborn. We had a hospital packing list that I wrote and rewrote for weeks. I wanted to be prepared. Nothing would catch me off-guard.
A few days after I got that first positive pregnancy test, I ran to my local Barnes & Noble to pick up a few books to help me prepare. Then I placed an Amazon order for a few more books. I bought books on pregnancy, breastfeeding, labor/delivery, pumping, and parenting skills. Initially, I struggled with some severe insomnia, so I spent many late nights googling and reading about every plausible scenario that could play out over the next nine months. I even made an illustrated guide on how to care for a newborn. We had a hospital packing list that I wrote and rewrote for weeks. I wanted to be prepared. Nothing would catch me off-guard.
Looking back, six months postpartum, I can only sigh and shake my head at how silly that had been.
My Journey With Postpartum Mental Illness
My son was born four weeks early and, after getting about an hour of skin-to-skin, they whisked him away to the NICU for 24-hour observation. I remember laying in the hospital bed, trying to focus on what the nurse was saying – something about standing up? – and only registering that I was shaky and scared. I had read that between 70-80% of mothers experience the baby blues, a temporary rollercoaster of your emotions as your hormones regulate postpartum.
I knew to expect some crying and even irritability. My OB had also already talked to me about my likelihood of developing postpartum depression (PPD) and postpartum anxiety (PPA). We had discussed how my generalized anxiety and depression increased my odds of a postpartum mental illness.
I believed I could handle whatever my brain threw at me.
Then the uncontrollable crying started on day two of our hospital stay. At a moment’s notice, I would suddenly be sobbing. Sometimes I would understand why (I needed to step away from my baby to shower and didn’t want to) and sometimes I was clueless. The anxiety came as a whole-body experience. I felt so out of control. I would hold my little five-pound, five-ounce son and wonder how I could cry when I made this beautiful boy.
Everyone reassured me it would be very short-lived. I did the breathing exercises. I texted my mom when the tears came. Two weeks came and went. The sleep deprivation acted as a fog in my brain. The night that my husband had gone back to work, the dreaded 11 pm – 7 am shift, I experienced my first intrusive thought. My son was crying and my brain could only think, “I just need him to shut up!” I stopped dead in my tracks, stepped back, and began sobbing. I didn’t mean that, did I? Where did that come from? As I sat down to feed him, tears streaking my face, I opened up the messenger for my OB’s office. I typed out a desperate message, barely able to see through the tears because surely this isn’t supposed to happen.
Asking for Help
I found that almost everyone’s response to my intense anxiety and sadness was “it’s normal.“ I would give a half-hearted smile and nod to this, all while wondering how on earth that could be true. How could it be normal to be so anxious you can’t sleep unless you’ve checked on the baby 12 times and kept the monitor three inches away, even though he’s asleep in a bassinet right next to you? How could it be normal to be terrified of driving because he’s definitely going to asphyxiate in his car seat, even though it’s set up exactly right? Or, how could it be normal to plant yourself on the couch with baby and boppy and simply not go anywhere because you’re safe there? If they are “normal,” they can’t be okay to leave unchecked, right? I want to be a healthy and present mom to my son.
In these moments of pure panic, logic evades me. Normally, I could absolutely remind myself that I installed the car seat per the manual and the little green level is perfectly set. He’s not going to asphyxiate. Then I remember that I saw somewhere online that asphyxia looks the same as sleeping and the moment he takes a nap on the way to my parent’s house, it’s game over for my anxiety. No amount of diaphragmatic breathing or calming phrases can pull me from the spiral. It’s a sudden assault on my brain by intrusive thoughts and the need to get my son to move some part of his little body or make a noise so that I know he’s alive. Until I see or hear that sign of life, the thought won’t leave. The anxiety sinks deeper into my skin.
 Six Months Postpartum
Six Months Postpartum
It’s been six months since my son was born. I’ve been in and out of medical offices, in search of solutions. Twice a month, I log into virtual therapy sessions. My antidepressants went from a baby dose of 50mg dose to 150mg. I’ve dabbled in support groups. Yet, I still spend most of the day floating between the couch, the kitchen, and my son’s pack-n-play for diaper changes. I keep my day as predictable as I can because it’s safe. I know what will happen. Sometimes, when I’m feeling really good and together, we will venture out to Target or pick up Starbucks. On my best days, we manage a walk with friends. Those days, however, are rare.
The fact that my son (knock on wood) has started sleeping longer stretches at night has really helped me feel less afraid of the day but I still feel like I’m moving through wet cement. I can’t walk from the nursery to the bedroom while holding my son without thinking, “What if we fell down the stairs right now? Who would save us?” I’ve entirely stopped leaving the house after 6:30 pm because the anxiety of messing up the bedtime routine is absolutely crippling.
The idea of transitioning my son to his crib from the bassinet next to my side of the bed makes me nauseous. I think about trying solid foods and then put the items back on the shelf at the store because what if he chokes and my sister, an EMT who lives with us, isn’t home when it happens? Here and there, I see little hints of postpartum OCD creep in. I see his sleep sack might be a bit too close to his chin and then I can’t go to sleep until I’ve checked, rechecked, and checked again that it’s positioned safely. Then, in my tired state, I’ll wonder if I actually checked adequately. So I’ll start over.
Most days are me functioning at the lowest level, praying my son doesn’t notice.
A month ago, I took my son to the pediatrician’s office for a weight check. I’d had this itch in the back of my brain for a while that he didn’t seem to be gaining much weight. We don’t have a reliable scale at home and I had been putting off making the drive over to the office. I stared in disbelief at the scale. He had only gained nine ounces in two months. We set up a follow-up with the doctor and a plan to supplement with formula after each nursing session. I smiled and thanked the nurses before leaving. Once I was in the car, I felt every part of me unravel and I began sobbing. This was my fault. My body, my milk, was failing my baby. He was already so small from being premature. I left a blubbering, panicked voicemail for my husband and then dialed my mom. I just needed someone to say I hadn’t been starving my son. In reality, it was a tongue and lip tie that were restricting his ability to get a good latch. Two weeks later, we got in with a wonderful ENT and had the ties revised. He healed wonderfully. He gained a ton of weight in the interim, happily chugging down every bottle. Did I know, logically, that I hadn’t been doing anything wrong? Did I know that the countless hours of nursing and sore nipples were worth something? Yes. In the moment, did the logic matter? Absolutely not. All I could think about was how this had to be all my fault.
Yesterday, he was weighed at his six-month well visit. We cheered at the two pounds he’d packed on in the past month. He just giggled at us, flapping his little arms.
 Still…sometimes I sit and stare at my son, banana teether shoved into his mouth and covered in drool, and feel like I’m still failing him. I had planned on being the fun, outgoing, makes homemade purees, DIYs new sensory activities every day, always trying something new mom.
Still…sometimes I sit and stare at my son, banana teether shoved into his mouth and covered in drool, and feel like I’m still failing him. I had planned on being the fun, outgoing, makes homemade purees, DIYs new sensory activities every day, always trying something new mom.
I wanted to be a source of light. Instead, I feel like I’ve let him down.
I haven’t made a single sensory activity for him, despite frozen peas sitting in the freezer for a month. (Apparently, you can throw them in a freezer bag of water for an engaging Tummy Time.) But even that feels like too much most days. I bulk-made purees one time. Then I completely dropped the ball and we’ve worked through only three of them. I wanted to be the Gentle Parenting mom – not the postpartum rage mom who feels her skin prickle and jaw clench when her son cries for more than a few minutes. There is so much that I feel just slipped through my fingers with becoming a mom who has postpartum mental health issues. I can’t help but think it wasn’t supposed to be like this.
I spend so much time wondering how our society can leave moms unprepared to manage our mental health while caring for a newborn and our healing bodies. I read about the night nurses, lengthy parental leave, and baby boxes provided to all new parents in other countries. France even provides you with a Carnet de santé – an actual baby manual. Denmark covers 90% of a parent’s wages for up to 32 weeks of leave. China has a custom for new mothers where they partake in a period of seclusion known as the “sitting the month” to aid in healing and milk production.
External support is even more important for moms who do not have family or friends who they can lean on. Having family nearby has been my saving grace throughout my struggle with PPA/PPD. Knowing my parents or sisters would be overjoyed to hang out with my son for a bit if I needed them to. Knowing that if the loneliness of being a stay-at-home mom started to get to me, I could just show up at my parents’ house without notice and be welcomed in with open arms. Then I can come home to a supportive spouse. I can text friends, a few of whom have babies one to three months older than my son, and vent about how I just need to shower without hearing phantom crying. My heart aches for those doing this entirely on their own. We get told our whole pregnancy that “It takes a village” and then so many moms never see anything resembling a village. Somewhere along the way, American society decided moms could and should do it all on their own – regardless of the consequences to our mental and physical well-being.
If you feel like you are in need of immediate help, please call 911 or your doctor’s office. If you’re in the Charleston area, visit Postpartum Support Charleston for information, local resources, and support groups. You can also find resources and support through Postpartum Support International.












